As of April 11, 2020, the Centers for Disease Control and Prevention (CDC) reports 492,416 cases of COVID-19 and 18,559 COVID-19-associated deaths. The United States now has the highest number of confirmed COVID-19 cases in the world. These numbers may be an underestimation of the true burden of the disease due to lack of testing and a high proportion of asymptomatic yet infectious individuals.
We urge everyone to continue to social distance: it is working!
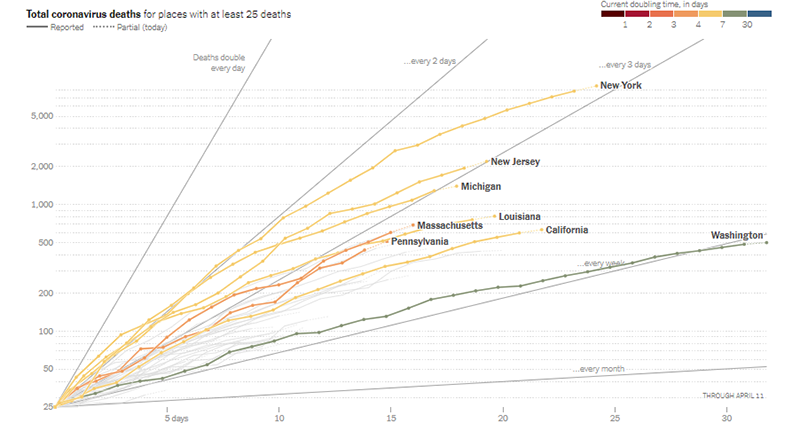
Washington and California quickly imposed statewide social distancing through stringent shelter-in-place or stay-at-home policies once deaths occurred within their borders. The graph below shows that COVID-19 deaths are still increasing in these two states, but not as fast as in other states. Deaths in New York State are now doubling every 3 days (when last week it was every 2 days), and in Washington State and some California counties, deaths are doubling only every week.
The most up-to-date version of the graph below can be accessed from the New York Times website here.
In this week’s update, we answer the following important questions:
- What types of treatments are available for COVID-19?
- If I suspect I have COVID-19, what should I do?
- If I had COVID-19 and have now recovered, will I become immune to SARS-CoV-2?
- Can I find out if I was naturally infected with SARS-CoV-2, the virus that causes COVID-19, and have developed immunity?
- How can I tell if information I read about COVID-19 is reliable?
1. What types of treatments or vaccines are available for COVID-19?
If you or your loved one (caregiver) has a confirmed diagnosis of COVID-19, your/their healthcare provider will be the right person to decide what type of treatment is useful. Please do not treat COVID-19-related symptoms without consulting your healthcare provider. Do not try to procure or hoard medications such as hydroxychloroquine that are approved for use in other conditions, as this is creating a shortage of these medications for patients with conditions for which the drugs are already approved.
Currently, no specific treatment or vaccine is available for COVID-19. This continues to be an area of intense investigation. Some of the drugs described below may be available to COVID-19 through compassionate access. This does not mean a drug is approved for the treatment of COVID-19. It is important to keep in mind that properly controlled clinical trials take a long time to conduct.
Treatment
Various compounds such as remdesivir and hydroxychloroquine are being studied for the treatment of COVID-19.
- Remdesivir is an antiviral drug. It has been shown to be active against a broad group of viruses such as filoviruses (cause of Ebola) and coronaviruses (eg, SARS-CoV and MERS-CoV). SARS-CoV is the cause of SARS and MERS-CoV is the cause of middle-east respiratory syndrome. These two viruses are related to SARS-CoV-2, the cause of COVID-19. Remdesivir has been shown to protect against infection and treat infection caused by these coronaviruses in preclinical models (experiments involving animal models of virus infection). A recent publication in the New England Journal of Medicine shows that remdesivir given to hospitalized COVID-19 patients helped improve symptoms. Though promising, it is important to note that this study included a small sample of patients. Randomized clinical studies with appropriate controls are necessary before remdesivir becomes approved for use with all COVID-19 patients.
- Hydroxychloroquine is a drug used to treat malaria and autoimmune disorders such as rheumatoid arthritis. It is known by the name Plaquenil in the US. Currently, evidence suggesting the successful use of hydroxychloroquine in COVID-19 patients is limited, and mostly anecdotal. Clinical trials studying the effect of hydroxychloroquine in the treatment of COVID-19 are ongoing. Despite the President’s ongoing endorsement of hydroxychloroquine as an effective treatment for COVID-19, concerns about its cardiac toxicities are growing, especially for people with underlying cardiovascular disease. Recent guidance issued by leading heart disease organizations recommends caution when treating COVID-19 with the combination of hydroxychloroquine and the antibiotic azithromycin in certain patients.
Vaccines
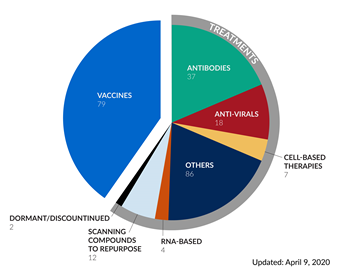
Historically, vaccines against viruses have been very effective in eradication of common viral diseases such as smallpox and polio. From an individual perspective, vaccination prevents or modifies the severity of a disease. From a public health perspective, a vaccine eliminates or eradicates a disease from the population (for example, smallpox). Since the SARS epidemic in 2003, several companies and institutions have already developed platforms for vaccine development against coronaviruses, which is a family of viruses that includes SARS-CoV-2, the causative agent of COVID-19. On January 23, 2020, the Coalition for Epidemic Preparedness Innovations (CEPI) was the first to announce funding of $12.5 million to develop vaccines against SARS-CoV-2 by three companies. Since then, both philanthropic and industry efforts have been mobilized for the development of a vaccine against SARS-CoV-2. As of April 9, 2020, there are close to 80 vaccine development efforts. It is important to keep in mind that vaccine development is a lengthy process and best-case estimates suggest that it will take a minimum of 18 months to deliver an effective vaccine against SARS-CoV-2. Even once a candidate vaccine is identified, it must be manufactured at scale for a global population. To speed these efforts, the Gates Foundation has announced that it is supporting construction of factories to pursue development of seven vaccine candidates.
Other treatments
Recently, the Bill & Melinda Gates Foundation also announced a $125 million partnership with Wellcome and Mastercard to accelerate the development of new drugs to treat SARS-CoV-2 infection. To track treatments that are being investigated for COVID-19, please check out the Milken Institute COVID-19 treatment and vaccine tracker. Here, you will also find information on clinical trials testing potential COVID-19 drugs/vaccines.
2. If I suspect I have COVID-19, what should I do?
If you (as a patient) or a loved one (a caregiver) exhibits the symptoms of COVID-19 (including but not limited to fever, dry cough, shortness of breath), immediately follow self-quarantine procedures. Immediately contact your healthcare provider (could be your primary care physician) about whether you need to get tested. Your healthcare provider will be able to guide you on next steps. The CDC and the Association of Public Health Laboratories maintain a list of laboratories that are currently conducting COVID-19 tests.
Please remember that you may not have symptoms even if you are infected with SARS-CoV-2. Social distancing is the only way to avoid getting infected with the virus. As a caregiver, please take extra precautions when you need to leave your house or apartment.
3. If I had COVID-19 and have now recovered, will I become immune to SARS-CoV-2?
The answer is – we do not know. When an individual is infected with a pathogen, such as bacteria or a virus, typically the body mounts an immune response. This is true even in individuals who remain asymptomatic. The immediate immune response ensures that the pathogen is eliminated from the body, and immunological memory (the basis of vaccination) ensures that if the body encounters the pathogen in the future, the immune system is ready to fight it off.
In the case of SARS-CoV-2, based on experience with other coronaviruses such as SARS-CoV and MERS-CoV, we believe that development of immunity will be highly individual-specific. Some individuals may develop high amounts of antibodies against SARS-CoV-2 while others may not. Furthermore, it is not currently clear whether a one-time infection with SARS-CoV-2 confers lifetime immunity against the virus. Scientists are still evaluating what level of immunity is needed to confer protection against future infections with SARS-CoV-2.
4. Can I find out if I was naturally infected with COVID-19 and have developed immunity?
The answer as of April 13, 2020 is - we do not know. In order to check if an individual has been infected with a pathogen, healthcare providers can conduct blood tests (also known as serological tests) to check for indicators of immunity. For example, if you received the MMR vaccine, the doctor can check if you have immunity against measles, mumps, and rubella by looking at antibody titers in your blood.
In the case of SARS-CoV-2, the goal is to develop such a blood test that will help identify:
- Which individuals have been naturally infected with SARS-CoV-2 and have recovered from the infection (even those individuals who were asymptomatic)
- Which individuals have developed immunity against SARS-CoV-2 after they received a vaccine when the vaccine becomes available
Currently, scientists are studying which antigens of the SARS-CoV-2 will be the most effective in generating immunity. Several groups are developing blood tests, and one test has been FDA approved (but is not yet publicly available). There is hope that such tests will become available within the next few months (and probably sooner in some places), and will be useful in guiding how quickly normal activities can resume.
5. How can I tell if information I read about COVID-19 is reliable?
In the era of COVID-19 when information is evolving rapidly—with new information being available daily—it is important to depend on trusted and reputable sources of information. You will encounter several sources of information such as:
- Print (newspapers such as New York Times, which also have online versions)
- Online-only platforms such as Slate and Buzzfeed
- Journal article websites
- Personal blogs and stories
It is incredibly important to verify sources of your information to ensure that we are not spreading false information, which not only can cause unnecessary panic but can be downright harmful (such as misinformation regarding drugs). A good resource that provides guidelines to evaluate health information can be found here.
Resources and Websites
- IASLC’s Guide to COVID-19 and Lung Cancer – https://www.lungcancernews.org/iaslcs-guide-to-covid-19-and-lung-cancer/
- The National Cancer Institute has a special website for COVID-19 and emergency preparedness. Coronavirus: What People with Cancer Should Know - https://www.cancer.gov/contact/emergency-preparedness/coronavirus
- We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC)
- Johns Hopkins Coronavirus Resource Center
- Interactive map of US COVID-19 cases by state
- The One-Two Punch: Cancer and COVID-19 (an important perspective for cancer patients)
- You can find information specific to your state or city or town on your health department’s website.
- Directory of state department of health websites
- Directory of local health department websites
- American Medical Association resources for healthcare providers
- If you cannot avoid air travel, check out “Dirtiest Places on Airplanes: How to Avoid Germs”