Finding lung cancer early, when it is easiest to treat, can save lives.
 To help you understand and share this information, you can view our free booklet and Lung Cancer Basics on lung cancer screening and early detection that summarize the detailed information in the following sections.
To help you understand and share this information, you can view our free booklet and Lung Cancer Basics on lung cancer screening and early detection that summarize the detailed information in the following sections.
Early detection of lung cancer is defined as strategies that can detect lung cancer at a stagethe extent of cancer in the body where surgery or stereotactic body radiation therapy (SBRT) can be offered with the goal of a cure. There are a number of factors that determine the outlook for any lung cancer patient in addition to when the lung cancer is detected, including the type of lung cancer, the patient's health in general, and the responsiveness of the patient's lung cancer to treatment. However, lung cancer is most easily and effectively treated when it is found at an early stage. Statistically, those with lung cancer caught early on have a much higher likelihood of surviving at least five years after diagnosis than those diagnosed when the lung cancer is more advanced.
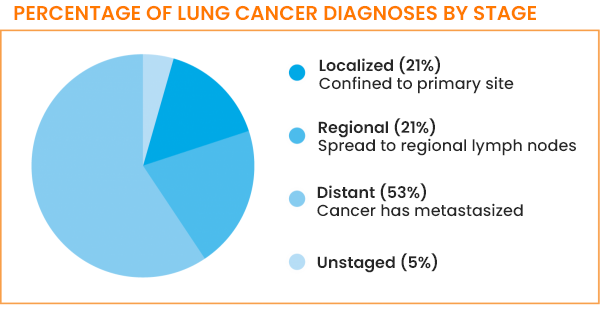
However, currently, only 21% of lung cancers are diagnosed while the tumor is still localized—that is, only found at the site where it started. This is commonly referred to as stage I. The major challenge is that most people with lung cancer only have symptoms when they are in later stages of the disease, so lung cancer is not usually suspected and discovered until it has had the chance to grow and spread.1
How can lung cancer be detected early?
Lung cancer can be detected early via screening.
Screening for lung cancer means checking for cancer before there are any symptoms. Examples of commonly used screening tests for cancer are mammograms for breast cancer, colonoscopies for colon cancer, and the PAP smear and human papillomavirus (HPV) tests for cervical cancer.2
For lung cancer, early-detection screening by a low-dose computed tomography (LDCT) scanA form of CT scan that uses less radiation than a standard chest CT (also called low-dose spiral CT scan or helical CT scan) has proven to be effective among individuals considered to be at high risk. It is also only recommended for these individuals. The usefulness of CT scans in high-risk individuals was demonstrated by the National Lung Screening Trial (NLST) and confirmed by the Nederlands-Leuvent Longkanker Screenings Onderzoek (NELSON) trial.
CT scans are much more sensitive than chest X-raysA type of radiation used in the diagnosis and treatment of cancer and other diseases and can detect smaller abnormalities that may be lung cancer. Chest X-rays are not recommended for lung cancer screening because they often miss early-stage lung cancers and have not resulted in decreased mortalityDeath rate, or the number of deaths in a certain group of people in a specific period of time. This is also the case for sputumMucus and other matter brought up from the lungs by coughing cytology, a test that checks for abnormal cells in sputum.3
Who should be screened for lung cancer?
There are several sets of guidelines, including the ones outlined below, to help determine who should be screened for lung cancer. These guidelines are primarily based on active (current or prior) tobacco exposure. The guidelines have been established in large part from the results of the National Lung Screening Trial (NLST). They are very similar, with the differences primarily related to the role of screening for the oldest patients and risk factors other than smoking. All of the patients who are recommended for screening are considered to be at high risk for developing lung cancer but do not currently have any symptoms to suggest that they do have lung cancer. Patients should discuss these guidelines with their doctor and understand the risks and benefits before undergoing lung cancer screening.
The guidelines from the US Preventive Services Task Force (USPSTF) include annual screening in adults who:11
- Are aged 50 to 80 years and
- Have a 20 pack-year smoking history and
- Currently smoke or have quit within the past 15 years

The USPSTF recommends that lung cancer screening stop once a person:11
- Reaches 81 years of age or
- Has not smoked in 15 years or
- Develops a health problem that substantially limits life expectancy or the ability or willingness to have curative lung surgery
The Centers for Medicare & Medicaid Services (CMS) covers costs associated with lung cancer screening based on the USPSTF criteria.
The guidelines from the National Comprehensive Cancer Network® (NCCN®) include annual screening for individuals in the following high-risk group. These are adults who:
- Are 50 years of age or older and
- Have a 20-pack-year or more history of smoking cigarettes
Follow-up screening may occur in 12 months, or sooner, depending on the recommendation of your healthcare provider.7
The guidelines from the American College of Chest Physicians (CHEST®) include annual screening with low-dose CT scans in adults as follows:8
Recommendation 1
- Are aged 55-77 years and
- Have smoked 30 pack-years or more and
- Either continue to smoke or have quit within the past 15 years
Recommendation 2
For asymptomatic individuals who do not meet the smoking and/or age criteria in recommendation 1 but:
- Are age 50-80 and
- Have smoked 20 pack-years or more and
- Either continue to smoke or have quit within the past 15 years
Recommendation 3
- For asymptomatic individuals who do not meet the smoking and/or age criteria in recommendations 1 and 2 but are projected to have a high net benefit from lung cancer screening based on the results of validated clinical risk prediction calculations and life expectancy estimates, or based on life-year gained calculations
What about screening for those who do not meet the current screening criteria?
Those who do not meet the current screening criteria should speak with their doctor about the current status of their eligibility for screening. Note that health insurance, both government and private, typically does not cover screening for those who do not meet the screening criteria.
The current criteria for lung cancer screening are based on active tobacco exposure. If you feel that you may have been exposed to other risk factors of lung cancer (read about risk factors here), you may choose to discuss the possibility of screening with your doctor.
What to expect during a low-dose CT (LDCT) screening scan
The low-dose CT scan is a computerized X-ray imaging procedure that yields detailed pictures, or scans, of areas inside the body. Because the scanning produces multiple images from different angles, it can show both two-dimensional (2D) and three-dimensional (3D) images of anything abnormal in the chest. CT scan images show more detail than a traditional X-ray.14
CT scans are a painless and noninvasive procedure; the patient needs no dyes or injections and has nothing to swallow.15
The scan itself takes less than a minute. During the procedure, the patient lies very still on the CT table. Depending on the scanner, either the table passes slowly through the center of the scanner or the table stays still while the scanner moves around the patient. There might be whirring sounds during the procedure. At times during the procedure, the technician operating the equipment will ask the patient to hold his or her breath; this prevents blurring of the images.14,15
A CT scan can provide very detailed information, including the size, shape, or location of an abnormality. However, a scan cannot diagnose whether or not an abnormality is cancer. What happens when a pulmonary nodule is found is discussed in a later section.

What else to know about lung cancer screening
Despite the benefits of low-dose CT scans for lung cancer screening, including decreased mortality from lung cancer, decreased mortality from lung cancer treatment, and improved quality of life, there are some drawbacks and risks, including that a CT scan may:6,14,16,17
- Find abnormalities that have to be checked with either another scan or a biopsyThe removal of cells or tissues for examination by a pathologist if considered suspicious; the vast majority of the time these end up not being cancerous
- Miss very small cancers or cancers that are hidden behind other structures in the chest
- Expose a patient to a small amount of radiation. While it is a smaller dose than that from a standard CT scan, multiple low-dose CT scans can lead to greater radiation exposure. High doses of radiation exposure can lead to other types of cancer in the future
- Detect tumors that would not become problematic. Such tumors may be indolent (tumors that grow slowly and may not always require treatment)
- Have costs for the patient that are not covered by the patient's insurance
- Cause stress while waiting for test results
In addition:
- Not all tumors that are found will be at an early stage
- Screening can only be done at facilities that can perform a low-dose CT scan, so a patient may have to travel to obtain a screening
It is important to keep in mind that a low-dose CT scan can find other abnormal growths in tissues outside the lungs (incidental nonpulmonary findings). These findings need to be followed up on by your doctor or specialist.
What is shared decision-making? Why is it important for lung cancer screening?
Ideally, the decision to be screened or not should be made together by the patient and the patient's primary care doctor or pulmonologist. The doctor knows the patient's history and possible risk factors best and can help guide the patient to the right screening center. (Some screening centers require a doctor's prescription in advance for a scan. Others will do an evaluation, also called a risk assessment, without a prescription to determine whether a patient's history and risk factors warrant a scan.)
In most cases, before screening is initiated, a face-to-face visit between you and your primary care doctor or pulmonologist is required. During this visit, the doctor will ask you for specific information relating to your current and past cigarette use, and together you will discuss the benefits and harms of CT lung screening and tobacco cessation counseling. This is termed a shared decision-making visit. Information gathered and documented in the office visit notes (medical record) will determine whether you are eligible for a low-dose CT scan lung screening program.18
Choosing a screening center
The National Comprehensive Cancer Network® recommends going to screening centers that:7
- Follow an organized plan that is updated to include new technology and knowledge
- Have a high-quality screening program with enough staff and resources
- Are accredited to do CT scans by a certifying organization, such as the American College of Radiology
- Get scans read by an American Board of Radiology board-certified radiologist who is an expert in lung cancer screening
- Offer modern multislice CT equipment (which is able to take multiple images in one rotation of the equipment) that does high-quality, low-dose, and non-contrast spiral CT scans
- Partner with a health center that has experience and excellence in biopsy methods, board-certified pulmonologists (lung doctors), and board-certified thoracic (chest) surgeons who are experts in lung cancer
What happens if a lung nodule is detected during lung cancer screening?
A low-dose CT scan can detect lung (pulmonary) nodules—small and roundish or oval growths of tissues in the lung that appear white—with great accuracy. However, a low-dose CT scan does not indicate whether the nodule is cancerous or not. Pulmonary nodules are associated with infectious and inflammatory diseases as well as with lung cancer. As discussed earlier, most pulmonary nodules are benign, that is, not cancerous.7,17
The first low-dose CT scan is known as the baseline screening. All scans after this, known as follow-up screenings, are compared with the baseline screening to determine whether there is a reason to suspect lung cancer. The patient's medical history, the characteristics of the nodule, and how fast the nodule grows determine follow-up care.
Based on whether a lung nodule is detected during the baseline screening, the National Comprehensive Cancer Network® recommends the following:7
If no nodule is detected at this screening, the next screening should be in 12 months, with additional follow-ups every 12 months after that. The doctor will determine how many follow-up screenings the patient needs.
If one or more nodules are detected at the baseline screening, additional tests (including a CT and/or a PET/CT scan to get a clear view of the nodules and what is going on throughout the body) or a follow-up low-dose CT scan sooner than 12 months may be indicated. The type of follow-up recommended—and the timing of follow-up—is based on several factors:
- Size: The larger the nodule, the sooner the follow-up is likely to be. Nodules with a diameter of 5 mm or less are of the least concern.
- Density: Density is how solid the nodule is, as determined by how well the X-rays from the LDCT pass through it. As discussed earlier, nodules that are solid and part-solid are of more concern for lung cancer than those that are nonsolid.
- Location: Nodules that are located in the upper lobes of the lung are more likely to be cancerous.
- Rate of growth: Nodules that grow faster are more likely to be cancerous. The growth rate of a nodule can be calculated by looking at the size of the nodule in follow-up scans.
- Medical history: The healthcare team considers the presence of risk factors of lung cancer, including age and family history of lung cancer.
If at baseline or at a follow-up scan, a nodule's characteristics make it of high concern for lung cancer, either a biopsy or surgical removal of the nodule will be done to confirm whether the nodule is cancerous. If the patient does have lung cancer, further tests may be needed to determine the stage.
For early-stage patients, treatment will be surgery or SBRT. For advanced-stage patients, treatment will begin, ideally after comprehensive biomarker testingAnalyzing DNA to look for gene mutations that can be treated with targeted therapy drugs and measuring the level of expression of the PD-L1 protein to determine the likelihood of a good response to immunotherapy drugs takes place and a personalized treatment plan is developed.
For detailed information about the National Comprehensive Cancer Network® guidelines for baseline and follow-up screenings, refer to NCCN® Guidelines for Patients: Lung Cancer Screening.
The American College of Radiology has developed a scoring system called Lung CT Screening Reporting & Data System® (Lung-RADS®) to standardize how results from CT scans are reported to reduce confusion in lung cancer screening CT interpretations and improve follow-up CT scans and care.19
The higher the score, the higher the probability of the nodule being cancerous and requiring follow-up. Not all low-dose CT scan results are reported in Lung-RADS® at this time.
Latest research in lung cancer screening
Advances in imaging techniques, such as the low-dose CT scan, have improved the chances of finding lung cancer early. Researchers continue to look for other techniques that could help identify lung cancer at an early stage. More sensitive tests that can find evidence of lung cancer in sputum or blood, even before the cancer is seen on a CT scan, are being studied.
Research is also being done on whether biomarker testing can identify which patients have a higher risk of lung cancer. There are many clinical trialsType of research study that tests how well new medical approaches in screening, prevention, diagnosis, or treatment work in people underway looking at these approaches to screening as well as others.
For detailed information about clinical trials and the potential benefits and risks of participating in one, read about them in Clinical Trials.
Updated February 12, 2024
References
- SEER Stat Fact Sheets: Lung and Bronchus Cancer. National Cancer Institute website. http://seer.cancer.gov/statfacts/html/lungb.html. Updated April 2023. Accessed February 5, 2024.
- Guidelines for the Early Detection of Cancer. American Cancer Society website. www.cancer.org/cancer/screening/american-cancer-society-guidelines-for-the-early-detection-of-cancer.html Revised November 1, 2023. Accessed February 5, 2024.
- Lung Cancer Screening. RadiologyInfo.com website. https://www.radiologyinfo.org/en/info.cfm?pg=screening-lung. Reviewed November 1, 2022. Accessed February 5, 2024.
- Aberle, DR, Adams AM, et al. Reduced Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med 2011; 365:395-409. doi: 10.1056/NEJMoa1102873. http://www.nejm.org/doi/full/10.1056/NEJMoa1102873#t=article. Published August 4, 2011. Accessed February 5, 2024.
- de Koning JH, van der Aalst CM, de Jong Pa,, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med. 2020:382(6):503-515. Accessed February 5, 2024.
- Lung Cancer Screening. US Preventive Services Task Force website. www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening. Published March 9, 2021. Accessed February 5, 2024.
- NCCN Guidelines for Patients®: Lung Cancer Screening, Version 2.2024. The National Comprehensive Cancer Network® website. www.nccn.org/patients/guidelines/content/PDF/lung_screening-patient.pdf Posted October 18, 2023. Accessed February 5, 2024.
- Mazzone PJ, Silvestri GA, et al. Screening for Lung Cancer: CHEST Guideline and Expert Panel Report. CHEST Journal. November 2021;160(5):E427-E494. journal.chestnet.org/article/S0012-3692(21)01307-6/fulltext Accessed February 5, 2024.
- Berg CD: Improving selection of individuals into lung cancer screening programmes. Lancet Oncol. 2019:20(8):1039-1040. Accessed February 5, 2024.
- Luo YH, Luo L, Wampfler JA, et al. 5-year overall survival in patients with lung cancer eligible or ineligible for screening according to US Preventive Services Task Force criteria: a prospective, observational cohort study. Lancet Oncol. 2019:20(8):1098-1108. Accessed February 5, 2024.
- Recommendations: Lung Cancer Screening. US Preventive Services Task Force website. www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening March 09, 2021. Accessed February 5, 2024.
- Mazzone PJ, Lam L. Evaluating the Patient With a Pulmonary Nodule: A Review. JAMA. 2022;327(3):264–273. doi:10.1001/jama.2021.24287. Accessed February 5, 2024.
- Pulmonary Nodules. Cleveland Clinic website. my.clevelandclinic.org/health/diseases/14799-pulmonary-nodules. Reviewed May 28, 2021. Accessed February 5, 2024.
- Computed Tomography (CT) Scans and Cancer. National Cancer Institute website. https://www.cancer.gov/about-cancer/diagnosis-staging/ct-scans-fact-sheet. Reviewed August 14, 2019. Accessed February 5, 2024.
- Low-Dose CT Scan for Lung Cancer Screening. Swedish Health Services website. https://www.swedish.org/services/thoracic-surgery/our-services/lung-cancer-screening-program/low-dose-ct-scan-for-lung-cancer-screening. Published 2022. Accessed February 5, 2024.
- National Lung Screening Trials: Questions and Answers. National Cancer Institute website. https://www.cancer.gov/types/lung/research/nlst. Updated September 8, 2014. Accessed February 5, 2024.
- Terpennings S, Lin CT, White C. Lung Cancer Screening: Pros and Cons. Applied Radiology website. http://appliedradiology.com/articles/lung-cancer-screening-pros-and-cons. Published July 1, 2015. Accessed February 5, 2024.
- CT Lung Cancer Screening: Shared Decision-Making Visit Requirements. American College of Radiology website. www.acr.org/-/media/ACR/NOINDEX/Advocacy/CT-LCS-shared-decision-making_fillable.pdf. Published 2019. Accessed February 5, 2024.
- Lung CT Screening Reporting & Data System (Lung-RADS). American College of Radiology website. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads. Published 2019. Accessed February 5, 2024.
