Small cell lung cancer (SCLC) accounts for about 15% of all lung cancers. In addition to existing treatment approaches, several promising new treatment approaches are being developed.
What is small cell lung cancer (SCLC)?
SCLC is one of the two major types of lung cancer. It differs from the other major type of lung cancer, non-small cell lung cancer (NSCLC), in a number of ways, including where the cancer begins, the way the cells appear under a microscope, and the way the cancer progresses.1,2,3
SCLC derives its name from the way the cancer cells look under a microscope; they are round, oval, or spindle-shaped and smaller than both normal, healthy cells and the cells of the different types of NSCLC. SCLC is sometimes also called small cell carcinoma or oat cell cancer.3
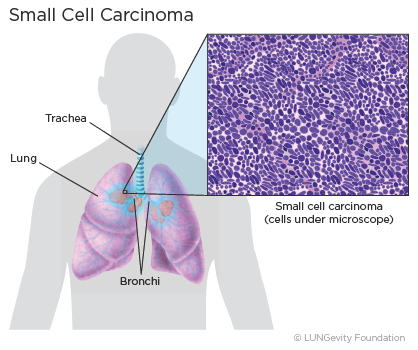
SCLC usually begins in the bronchiThe large air passages that lead from the trachea (windpipe) to the lungs, the major airways in the center of the chest that lead to the lungs, although about 5% of the time it is found in the periphery of the lungs. SCLC is a type of neuroendocrine tumor. It is a very aggressive cancer that grows and spreads rapidly.1,2,
SCLC accounts for about 15% of all lung cancers, and is found most often in people with a smoking history.1,4
For more information about the signs and symptoms that might indicate SCLC, see the Signs & Symptoms section. Note that SCLC may not cause any symptoms, especially early in its development, and that the signs and symptoms are not specific to SCLC and may be caused by other conditions.
Diagnosing small cell lung cancer (SCLC)
Diagnosing lung cancer is a complex process. In addition to determining whether a patient has lung cancer, diagnosing includes categorizing lung cancers in ways that help to determine the best treatment plan.
How is small cell lung cancer diagnosed?
Different tests are used to diagnose lung cancer and determine whether it has spread to other parts of the body. Some of these tests can also help to decide which treatments might work best. Steps and tests used in diagnosing SCLC may include:
- Imaging tests
- Biopsies (A tissue biopsy is the only way to confirm a diagnosis of lung cancer.)
The diagnostic approaches used for an individual will depend on medical history and condition, symptoms, location of the nodule(s), and other laboratory test results.
For more information about the different steps and tests for making a lung cancer diagnosis, see the Diagnosing Lung Cancer section.
Stages of lung cancer
Staging is a way of describing where the cancer is located, if or where it has spread, and whether it is affecting other parts of the body. Doctors use diagnostics to determine the cancer’s stage, so staging may not be complete until all of the tests are finished. Knowing the stage helps the healthcare team:
- Understand how advanced your lung cancer is
- Recommend those treatments that are likely to be the most effective
- Evaluate your response to treatment
SCLC is treatable at any stage.
Staging of SCLC is described in two different ways:
- Traditionally, the two-stage Veterans Administration (VA) classification system has been used for SCLC:2,3,5,6
- Limited-stage means the cancer is only in one side of the chest: one lung, the tissues between the lungs, and nearby lymph nodes only. About one-third of those diagnosed with small cell lung cancer have limited-stage disease at the time of their diagnosis.
- Extensive-stage means the cancer has spread widely through a lung, to the other lung, to lymph nodes on the other side of the chest, or to distant organs. Many doctors also describe cancer that has spread to the fluid as extensive-stage.
- More recently, the same system that is used for NSCLC is being used either alone or in combination with the two-stage VA classification system because it helps with treatment decisions:2,3,7,8,9,10,11
- A number from one through four (I, II, III, or IV), where IV represents the most advanced cancer, based on the TNM system, where staging is based on the values assigned to a patient's lung cancer based on three criteria: T (tumor), N (node), and M (metastasis).
- Stages I, II, and III of the TMN system correspond with limited-stage in the VA system, while stage IV corresponds with extensive-stage. In both Stage IV and extensive-stage small, the cancer is metatstatic.
Current National Comprehensive Cancer Network (NCCN) guidelines recommend the dual approach to staging SCLC.2
For more information about how stages are determined and the chararacterisics of each stage,see the Lung Cancer Staging section.
Driver mutations
A patient's SCLC may or may not have one of the known driver mutations—changes in a patient's DNA that lead to small cell lung cancer or cause it to progress. Known driver mutations in SCLC include TP53 and RB1, the two most prevalent.12 In biomarker testing (also called mutation, genomic, or molecular testing), the patient's DNA is analyzed to determine whether any of these driver mutations is present. For NSCLC, there are treatments that target several of the driver mutations, so biomarker testing is recommended. However, this is not yet the case for SCLC. There are currently no U.S. Food and Drug Administration (FDA)-approved treatments for any of the known small cell driver mutations.
At this time, biomarker testing is not recommended in general for SCLC patients; however, a patient's healthcare team may recommend biomarker testing if the patient is considering participating in a clinical trial for a drug that targets a small cell driver mutation.
Treatment options for small cell lung cancer (SCLC)
There are a number of treatment options for SCLC. Which ones are used to treat a specific patient’s lung cancer will depend on the stage of the cancer, the patient’s overall health, including how well the organs of the patient's body are functioning, and the patient's preferences. (A patient's age alone does not predict whether a patient will benefit from treatment.)3,5
Patients may be as involved in the treatment plan decision as they want to be. Patients should discuss all of the options, understand what the goal of each option is (for example, cure vs. control), consider the benefits and risks of each, check about likely side effects, understand how everyday life might be affected, find out what the treatment will mean financially, and not hesitate to get a second opinion if there are unaddressed concerns.13,14
It is always a good idea for a patient to take someone along to appointments to help with questions and take notes.
What are currently approved treatment options?
Approved treatment options for SCLC include:
- Surgery
- Radiation therapy
- Chemotherapy
- Immunotherapy
The US Food and Drug Administration (FDA) has approved three immunotherapy drugs for the treatment of patients with metastatic (extensive-stage or stage IV) SCLC under various conditions and one immunotherapy drug for limited-stage SCLC.
For more information about approved treatment options for small cell lung cancer by stage, see the Treatment Options for Small Cell Lung Cancer by Stage section.
Surgery
Surgery is a treatment option for only a small percentage of limited-stage SCLC patients. It appears to be effective only among the less than 5% of patients whose limited-stage cancer is also stages 1-IIA cancer, in which the tumors are small (no larger than 5 cm across) and have not spread to lymph nodes.3
If surgery is performed, lobectomy, in which the lobe of the lung where the tumor is located is removed, is the preferred type of surgery.3
The surgery is followed up with adjuvant chemotherapy or a combination of chemotherapy and radiation therapy.3
Read more about different surgical options, when they are used, and what to expect after surgery in the Treatment Options: Surgery section.
Radiation therapy
Radiation therapy is a type of cancer treatment that uses high-powered energy waves to kill cancer cells. The type of radiation therapy most often used for treating SCLC is external beam radiation therapy (EBRT), which delivers radiation from outside the body.
Radiation therapy is used in two ways for limited-stage SCLC. The first way is as concurrent treatment with combination chemotherapy. When used like this, the radiation therapy most often used for treating SCLC is external beam radiation therapy (EBRT), which delivers radiation from outside the body.3,15,16
The second way radiation therapy is used is called prophylactic cranial irradiation. For those limited-stage SCLC patients whose cancer has shrunk after treatment, radiation to the brain may be used because it reduces the risk of the cancer spreading there.3,15,16
For extensive-stage SCLC patients who have responded to the combination chemotherapy, both thoracic radiation therapy and prophylactic cranial irradiation may be used. Radiation therapy may also be used as a palliative treatment for extensive-stage SCLC.3,15
For those patients whose cancer has returned, palliative radiation therapy may be used to ease symptoms.3,15,16
For more information about radiation therapy, including how it works, how and when it is given, the different kinds, and common side effects, see the Treatment Options: Radiation Therapy section.
Chemotherapy
Chemotherapy is a systemic drug treatment, most often given intravenously to lung cancer patients, that targets and kills the rapidly growing cancer cells by traveling through the blood to reach the cancer cells wherever they are. Chemotherapy is the only treatment that is a component of the treatment plan for all SCLC patients.3,15,17,18
For most patients with either limited-stage or extensive-stage SCLC, the chemotherapy regimen most often used is a platinum-based chemotherapy drug, cisplatin (Platinol® or Platinol-AQ®) or carboplatin (Paraplatin®), in combination with etoposide (Etopophos®). Other combinations may be used as well. These include a combination of chemotherapy and immunotherapy for extensive-stage patients.3,15
SCLC patients tend to have a good initial reponse to chemotherapy, but the disease inevitably recurs (comes back) because resistance to the treatment develops. When it recurs, a single chemotherapy drug, such as lurbinectedin (ZepzelcaTM) or topotecan (Hycamtin®) may be used.2,3
Thoracic radiation therapy, as discussed earlier, is typically given together with chemotherapy for limited-stage SCLC. If the patient cannot tolerate radiation therapy, combination chemotherapy may be used alone. Some patients with extensive-stage disease may also be considered for thoracic radiation if they have a good response to their initial therapy and if their cancer is primarily active in the lungs and chest.3
For more information about chemotherapy, including how it works, how and when it is given, and possible side effects and how to manage them, see the Treatment Options: Chemotherapy section.
Immunotherapy
Immunotherapy is a type of therapy that increases the natural ability of the patient's immune system to fight cancer. Instead of trying to stop or kill the patient's cancer cells directly, as most other cancer treatments do, immunotherapy trains the patient's own natual immune system to recognize cancer cells and selectively target and kill them.19
The U.S. Food and Drug Administration (FDA) has approved two immunotherapy drugs for the treatment of patients with metastatic (extensive-stage or stage IV) SCLC under various conditions.
For more information about immunotherapy, including how it works, how and when it is given, and possible side effects and how to manage them, see the Treatment Options: Immunotherapy section.
Finding a clinical trial that might be right for you
Clinical trials are research studies among patients to find out whether new medical approaches that are being developed are safe and effective and better than those currently being used.
In addition to the approved treatments described above, researchers are testing several new types of treatment in clinical trials for people with small cell lung cancer, including targeted therapy and immunotherapy treatments among others.20 Clinical trials are considered a good option for small cell lung cancer patients, per NCCN guidelines.
Patients considering participating in a clinical trial should start by asking their healthcare team whether there is one that might be a good match for them in their geographic area.
For more information about clinical trials and resources for finding one, see the Clinical Trials section.
Managing symptoms and side effects
Lung cancer treatments can cause side effects. Side effects from lung cancer treatment are common, but just because a side effect is common does not mean that a patient will experience it. Before treatment begins for small cell lung cancer, patients should discuss with their healthcare team what side effects might be expected and how to prevent or ease them. Patients should also speak with their healthcare team if and when new side effects begin, as treating them early on is often more effective than trying to treat them once they have already become severe. Although most side effects go away when treatment is over, some can last a long time.
In addition to the side effects of lung cancer treatments, lung cancer itelf can result in a number of symptoms. For more information about the symptoms of lung cancer, see the Signs & Symptoms section.
Tips for managing specific symptoms and side effects related to treatment can be found in the For Supporters & Advocates section of the website, along with other practical and supportive resources for patients/survivors and caregivers.
To help reduce the severity and duration of most side effects and alleviate the cancer’s symptoms, a patient may want to request palliative care, also called “supportive care” or “symptom management.” There is sometimes confusion about the difference between palliative care and hospice care. Hospice care is a form of palliative care given only to patients whose life expectancy is six months or less. On the other hand, palliative care in general is an extra layer of support that can be initiated alongside other standard medical care. In fact, scientific evidence is starting to emerge that shows that palliative care may actually help patients live longer.
For more information about how palliative care can improve quality of life from the time of diagnosis, see the Palliative Care section.
The healthcare team
There are a number of doctors and other medical professionals who diagnose and treat patients with lung cancer. Together, they make up the comprehensive medical or healthcare team that patients see over the course of their care. Members of the healthcare team work together to provide care for a patient, including diagnosis, treatment, and side-effect management and other support services.
For more information about what each member of a healthcare team does, see the Your Medical Team section.
Patient Gateway: Living with small cell lung cancer
The Small Cell Lung Cancer Patient Gateway is the central hub for updates on treatment options, research news, and patient resources designed to help people live better with small cell lung cancer.
Updated December 12, 2024
References
- Wistuba I, Brambilla E, Noguchi M. Chapter 17: Classic Anatomic Pathology and Lung Cancer. In: Pass HI, Ball D, Scagliotti GV, eds. IASLC Thoracic Oncology, Second Edition. Philadelphia, PA: Elsevier; 2018: 143-163. Accessed February 5, 2024.
- Kalemkerian G, Schneider B. Advances in Small Cell Lung Cancer. Hematol Oncol Clin North Am. 2017:31:143-145. Accessed February 5, 2024.
- NCCN Clinical Practice Guidelines to Oncology (NCCN Guidelines®): Small Cell Lung Cancer. The National Comprehensive Cancer Network, Inc. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Version 1.2024– December 21, 2023. Accessed February 5, 2024.
- Lung Cancer — Small Cell: Risk Factors and Prevention. Cancer.Net website. https://www.cancer.net/cancer-types/lung-cancer-small-cell/risk-factors-and-prevention. Approved September 2022. Accessed February 5, 2024.
- Lung Cancer — Small Cell: Stages. Cancer.Net website. https://www.cancer.net/cancer-types/lung-cancer-small-cell/stages. Approved September 2022. Accessed February 5, 2024.
- NCI Dictionary of Cancer Terms. National Cancer Institute website. https://www.cancer.gov/publications/dictionaries/cancer-terms. Accessed February 5, 2024.
- Non-Small Cell Lung Cancer Stages. American Cancer Society website. https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/staging-nsclc.html. Revised November 20, 2023. Accessed February 5, 2024.
- Lung Cancer - Non-Small Cell: Stages. Cancer.Net website. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/stages. Approved December 2022. Accessed February 5, 2024.
- Detterbeck FC, Boffaa DJ, Kim AW, Tanoue LT. The Eighth Edition Lung Cancer Stage Classification. Chest, 2017; 151(1): 193-203. https://pubmed.ncbi.nlm.nih.gov/27780786/ Accessed February 5, 2024.
- Kay F, Kandathil A, Batra K, Saboo SS, Abbara S, Rajah P. Revisions to the Tumor, Node, Metastasis staging of lung cancer (8th edition): Rationale, radiologic findings and clinical implications. World J Radiol. 2017;9(6):269-279. Accessed February 5, 2024
- Rami-Porta R, Asamura H, Travis WD, Rusch VW. Lung cancer - major changes in the American Joint Commiittee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(2):138-155. https://pubmed.ncbi.nlm.nih.gov/28140453/ Accessed February 5, 2024.
- Byers L, Rudin C. Small Cell Lung Cancer: Where do we go from here? Cancer. 2015 Mar 1.; 121(5): 664-672. doi: 10.1012/cncr.29098. https://pubmed.ncbi.nlm.nih.gov/25336398/ Accessed February 5, 2024.
- Making Decisions about Cancer Treatment. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/making-decisions-about-cancer-treatment. Approved October 2022. Accessed February 5, 2024.
- Cancer treatment decisions: 5 steps to help you decide. Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/cancer/in-depth/cancer-treatment/art-20047350. Updated September 13, 2022. Accessed February 5, 2024.
- Lung Cancer – Small Cell Types of Treatment. Cancer.Net website. http://www.cancer.net/cancer-types/lung-cancer-small-cell/types-treatment. https://www.cancer.net/cancer-types/lung-cancer-small-cell/types-treatment. Approved September 2022. Accessed February 5, 2024.
- Radiation Therapy for Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/lung-cancer/treating-small-cell/radiation-therapy.html. Revised November 22, 2023. Accessed February 5, 2024.
- How is Chemotherapy Given? Chemocare.com website. https://chemocare.com/chemotherapy/what-is-chemotherapy/how-chemotherapy-is-given.aspx. Accessed February 5, 2024.
- Chemotherapy for Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/lung-cancer/treating-small-cell/chemotherapy.html. Revised November 22, 2023. Accessed February 5, 2024.
- Immunotherapy to Treat Cancer. National Cancer Institute. https://www.cancer.gov/about-cancer/treatment/types/immunotherapy. Updated September 24, 2019. Accessed February 5, 2024.
- ClinicalTrials.gov. US National Institutes of Health website. http://clinicaltrials.gov. Accessed February 5, 2024.
