As of June 12, 2020, the United States has reported more than 2 million cases of COVID-19, and 113,914 have died from this disease. States are in different phases of reopening and shelter-in-place restrictions, and lockdown have been eased in almost every state in the US. With restrictions being lifted despite the upsurge in new cases, a big question remains.
Is it safe to return to routine activities? The short answer to this question is NO – we are not yet ready to return to routine activities.
In this week’s update, we provide evidence on why the lung cancer community needs to be vigilant about the risk of exposure to SARS-CoV-2, the virus that causes COVID-19. We also describe the impact of easing shelter-in-place restrictions in different states in the US and conclude by providing expert guidance from epidemiologists on what to expect over the next year.
1. Lung cancer patients are at higher risk of developing complications from COVID-19: The Thoracic cancERs international coVid 19 cOLlaboraTion (TERAVOLT) registry study is specifically tracking outcomes for lung cancer patients infected with COVID-19. Recently published data from this study suggests that stage IV non-small cell lung cancer (NSCLC) patients are at higher risk of complications and mortality if they get infected with SARS-CoV-2. Of the patients included in the study, 33% succumbed to complications from COVID-19. Though the data generated for this study is primarily from European countries, it is highly probable the findings will hold true in other high-income countries such as the United States. Though the study does not provide information on the outcomes of small cell lung cancer (SCLC) patients, we anticipate that the findings will hold true for SCLC as well, given the high symptom burden of SCLC. Also, the TERAVOLT study has identified smoking history as an important predictor of developing complications from COVID-19. This suggests that SCLC patients may be at higher risk of a severe form of COVID-19, given the association of SCLC with active tobacco exposure.
It is important to keep in mind that the CDC considers patients with lung co-morbidities (such as lung cancer) to be at a higher risk of developing complications from COVID-19.
2. Easing shelter-in-place restrictions has led to an escalation in new COVID-19 cases in the United States: It is now proven that public health measures such as home isolation, business closures, and other large-scale social distancing measures have had large and measurable health benefits in containing the spread of COVID-19 and “flattening the curve”, as described by a recent research study in the journal Nature. Therefore, before lifting or removing these restrictions, there needs to be careful deliberation taking into account the local case load of COVID-19 and availability of critical hospital resources, should there be a spike in cases when restrictions are lifted. In order to assist states in reopening, the CDC has suggested a phased approach to easing shelter-in-place restrictions. However, it is becoming increasingly apparent that we will need to monitor reopening with caution and continue to maintain public health precautions.
- The state of Florida reported a spike in COVID-19 cases since the state entered phase 2 reopening on June 5. The 64 counties that moved into the second phase of reopening saw a near 42% increase in new cases the week before that could not be explained by increased testing alone.
- The state of Arizona has seen a huge spike in the number of COVID-19 cases since the state eased restrictions at the end of May. Arizona’s Department of Health Services has reported that the state has already reached 80% of its ICU bed capacity.
If you are curious to see how your state is performing in light of the recent lifting of shelter-in-place restrictions, please check out this article.
3. We should continue to maintain public health measures to minimize exposure to SARS-CoV-2: Easing shelter-in-place restrictions does not mean we should stop maintaining public health precautions. We highly recommend that everyone:
- Wear masks in public. A recent publication in the Proceedings of the National Academy of Sciences shows wearing masks is protective, given that transmission of the virus through air is one of the primary means of infection.
- Continue to maintain six feet distance from others in public
- Continue to practice social distancing
- Self-quarantine in case you suspect you may have been exposed to the virus
- Wash your hands regularly with soap and water
- Avoid touching your face
- Avoid large gatherings of people
- Minimize all non-essential travel
As a lung cancer patient or caregiver, if you have any questions on how to maintain public health measures as you run errands and go to work, please check out the CDC resources here. We are also learning about the long-term effects of an infection. Impact of COVID-19 on the body can last for several months. In some extreme cases, damage to the lungs is severe enough to require a double-lung transplant. We therefore firmly believe that it’s better to be safe than sorry!
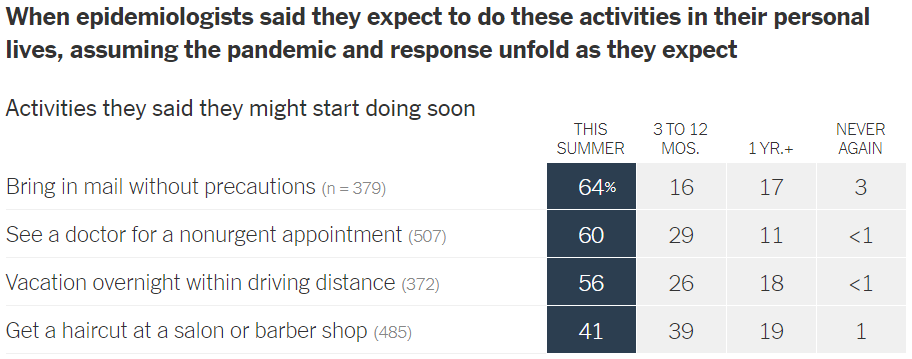
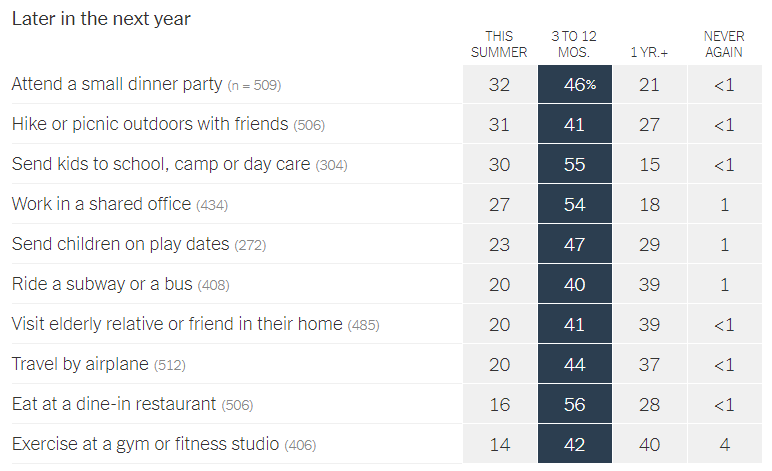
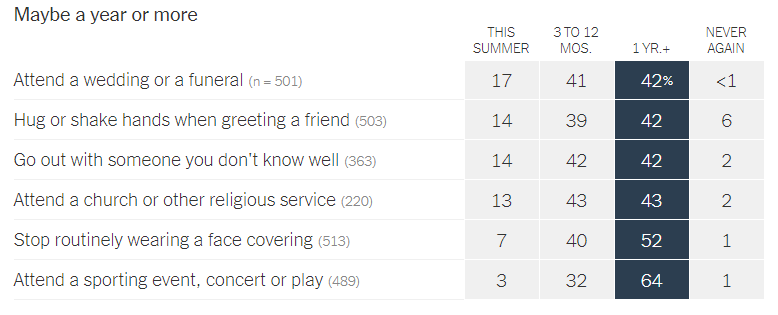
4. Epidemiologists suggest that the timeline for resuming different activities will be determined by the availability of a vaccine against SARS-CoV-2: In a recent article in the New York Times, 511 epidemiologists were asked to rate how soon they would resume different activities. Below are the results of this opinion survey. Though this data is not meant to serve as guidelines for the general public, it gives us a picture of where expert opinion lies with regard to when to resume normal activities.
Resources and websites
- IASLC’s Guide to COVID-19 and Lung Cancer
- The National Cancer Institute has a special website for COVID-19 and emergency preparedness. COVID-19: What People with Cancer Should Know
- We are following updates provided by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC)
- Johns Hopkins COVID-19 Resource Center
- Interactive map of US COVID-19 cases by state
- The One-Two Punch: Cancer And COVID-19 (an important perspective for cancer patients)
- You can find information specific to your state or city or town on your health department’s website.
- American Medical Association resources for healthcare providers.