Surgery—the removal of a tumor and some healthy tissue around the tumor during an operation—is a treatment option in lung cancer only when the patient is healthy enough for surgery, and the tumorAn abnormal mass of tissue that results when cells divide more than they should or do not die when they should:
- has been found early,
- is able to be completely removed safely, and
- has not spread within the chest or to other organs
When surgery is an option in a patient with non-small cell lung cancer (NSCLC)A group of lung cancers that are named for the kinds of cells found in the cancer and how the cells look under a microscope; the most common kind of lung cancer, it is the main treatment because it provides the best chance for a cure. Surgery can be used for NSCLC patients with stage I, stage II, and some stage IIIA lung cancers. It is not used for stages IIIB and Stage IIIC lung cancers, or for stage IV NSCLC, which is metastatic.1,2
Surgery is rarely used as the main treatment in small cell lung cancer (SCLC)A fast-growing cancer that forms in tissues of the lung and can spread to other parts of the body because most patients are diagnosed after the cancer has spread to other parts of the body.3
Lung cancer surgery may be used in combination with chemotherapyTreatment with drugs that kill cancer cells and/or radiation therapyThe use of high-energy radiation from x-rays, gamma rays, neutrons, protons, and other sources to kill cancer cells and shrink tumors. Chemotherapy and radiation therapy may be given either before surgery (neoadjuvantTreatment given prior to the main treatment in order to shrink a tumor) (for NSCLC stage IIIA lung cancer patients) or after surgery (adjuvantCancer treatment given after the primary treatment in order to kill unseen cancer cells or to lower the risk that the cancer will come back) for all NSCLC patients who undergo surgery, in order to eliminate any small amount of cancer that was not detected and removed by surgery.1,2,3
Patients should discuss with their healthcare team whether surgery is the best option for them. Lung cancer surgery is a complex operation that can have serious consequences. Therefore, it should be performed by a thoracic surgeon—a surgeon specially trained in operating on people with lung cancer. Patients often seek a second opinion with a thoracic surgeon when considering surgery.4
What is the goal of surgery in the treatment of lung cancer?
The goal of lung cancer surgery is to completely remove the lung tumor. The tumor is removed along with a border, known as a margin, of healthy tissue surrounding the tumor. The tumor is said to have clear margins if the pathologist who examines the tumor tissue after the surgery finds no cancer in the margin.
During surgery, nearby lymph nodesA rounded mass of lymphatic tissue surrounded by a capsule of connective tissue in the lung and middle portion of the chest are also removed to check them for cancer and to help determine whether further treatment is necessary.4
What are the different types of surgery used in lung cancer?
The type of surgery the thoracic surgeon recommends depends on the size and location of the tumor and on how well the patient’s lungs are working. If a patient’s lungs are healthy, a lobectomy is most commonly the preferred operation.5
Following are descriptions of different approaches that may be used:2,4,5,6,7
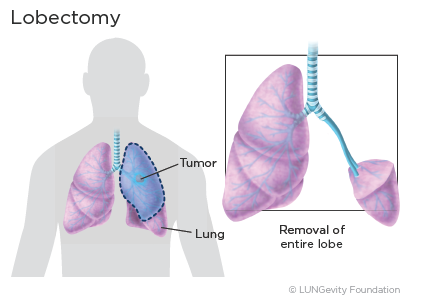
Lobectomy
Lobectomy is the removal of one of the five lobesA portion of an organ of the lung. When non-small cell lung cancer (NSCLC) is detected at an early stage, a lobectomy is the most effective type of surgery, even when the lung tumor is very small.
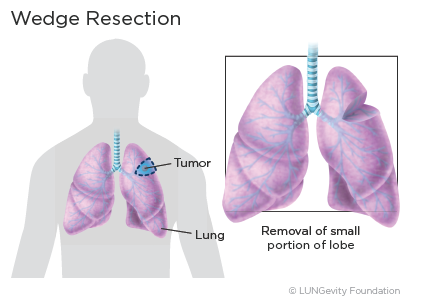
Wedge resection
In a wedge resection, the surgeon removes the tumor and a small rim of normal, healthy tissue surrounding it. A wedge resection is recommended for treating the smallest lung cancers (2 cm or less in diameter) or if the patient has poor lung function and/or other medical conditions that make removing the entire lobe dangerous. A wedge resection may also be performed if the patient has a peripheralAt the outermost part or region within a precise boundary lesion.
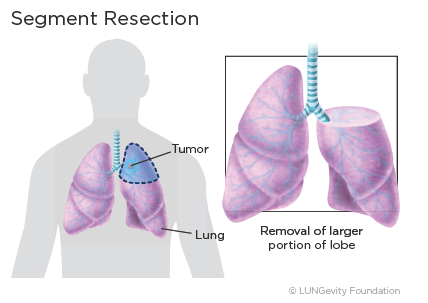
Segmentectomy
A segmentectomy removes one of the small segments within the lobes of the lung that contains a cancer. The amount of lung tissue removed is between what is removed in a lobectomy and in a wedge resection. Like wedge resection, it is recommended only for treating lung tumors that are 2 cm or less wide or, as with wedge resections, if the patient has poor lung function and/or other medical conditions that make removing the entire lobe dangerous.
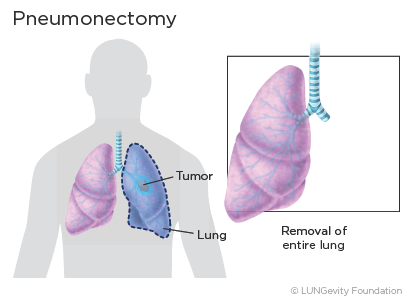
Pneumonectomy
Pneumonectomy is the surgical removal of the entire lung. This type of surgery is usually required if the tumor is very large or is close to the center of the chest.
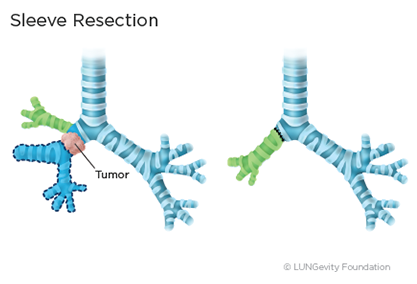
Sleeve resection
This surgery is used for tumors that involve the large airways. The tumor and a portion of the airway are removed and the ends of the airway are rejoined so remaining lobes can be left in place. A surgeon may perform this type of surgery rather than a pneumonectomy in order to preserve more lung function.
What are the different techniques used to perform lung surgery?
Thoracotomy
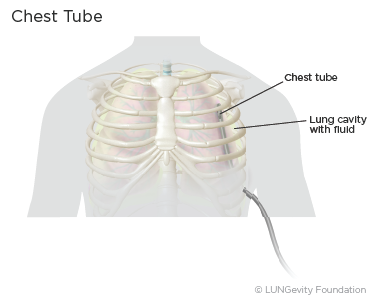
This surgery is performed in an operating room with general anesthesiaMedicine that puts the patient in a deep sleep. The surgeon makes an incisionA cut made in the body to perform surgery between the ribs on the side of the chest or on the back in order to examine the lung and remove the tumor, surrounding tissue, and nearby lymph nodes. After the surgery, a patient will have a tube (or tubes) coming out of the chest to drain excess fluid and air from the space around the lung while the lung heals. Once the fluid drainage and air leak subside, the tube(s) will be removed. Generally, the hospital stay after a thoracotomy is 5 to 7 days, followed by a period of recovery at home.8,9
Thoracoscopy
A thoracoscopy is a minimally invasive surgery that uses small incisions and small instruments to examine and perform operations in the inside of the chest. It is also known as video-assisted thoracic surgery, or VATS. This procedure requires a great deal of technical skill and should only be performed by a surgeon who has specific training and experience in it.
VATS to remove lung cancer is done in an operating room under general anesthesia. During the operation, a thin tube with a light and a tiny video camera on the end is placed through a small incision on the side of the chest. The view inside the chest is transmitted onto a television monitor. The surgeon can look around freely inside the chest, watching the image on the TV screen. One or two other small incisions are used for long instruments that are used to do the same operation that would be done using a thoracotomy. If a lobectomy or pneumonectomy is done, one of the incisions will be enlarged to allow the tumor and lung tissue to be removed.5,9
Since only small incisions are needed in a VATS, there is less pain after the surgery and a more rapid recovery. Chest tubes are required for most VATS procedures, and patients typically remain in the hospital for a few days until the drainage of fluid and air subsides. Research has shown that the cure rate after a VATS is similar to surgery done with a thoracotomy. However, less pain, fewer complications, and shorter hospital stays—four or five days—have been found with VATS.5,9
Robotic-Assisted Surgery
A newer type of minimally invasive operation known as robotic-assisted surgery is being performed at some large cancer centers in the U.S. In this approach, a surgeon sits at a control panel, inside the operating room, using robotic arms to maneuver the surgical instruments. Robotic surgery requires special training and expertise. Results from robotic-assisted lung cancer operations have been found to be comparable to those from VATS.9,10,11
What determines the length of the hospital stay after lung cancer surgery?
How long a patient needs to stay in the hospital after surgery will depend on:12
- Which type of surgery was done
- The patient's overall health before surgery
- The patient's lung function after surgery
- Post-surgical complications, if any
How can patients manage the effects of lung cancer surgery side effects?
Side effects from lung cancer surgery are common, but just becaus a side effect is common does not mean that a patient will experience it. Before surgery, a patient discuss with their healthcare team what side effects they might expect and lhow to prevent or ease them. A patient should speak with their healthcare team if and when new side effects begin, as treating them early on is often more effective than trying to treat them once they have already become severe. Although some side effects go away quickly, others may last a long time. The side effects and management techniques below are not all-inclusive. A patient's healthcare team will have a more extensive set of side effects and management recommendations.
Common side effects and management techniques for lung cancer surgery may include:
- Pain: Depending on the type of surgery a patient undergoes and how big the incision, the patient's chest and back may be painful for several weeks or longer after surgery. Pain medicines that will help can be prescribed.12 In addition, there are other other things that patients can do once at home to help lessen the pain; see Living Well With Lung Cancer.
- Fatigue: A patient should expect to feel more tired than usual after surgery. How long it will take to get back to normal is different for each patient. Rest is very important to recovery.13,14
- Fluid, blood, or air in the chest: One or more chest tubes are typically placed during surgery to keep the patient's chest cavity free of fluid, blood, and air that collect after lung surgery. The tubes will be connected to a machine that gently suctions the fluid from the chest. These tubes are left in place until the fluid and air have stopped draining. Air leaks typically stop 1-4 days post-surgery.12,15
- Shortness of breath:
 A patient should expect to feel short of breath after lung surgery. The extent of this depends on how much of the lung was removed and how much pain the patient is experiencing. After a portion of a lung is removed, the remaining lung tissue can expand over time and make it easier to breathe. A respiratory therapist can help the patient with breathing treatments after surgery. These treatments may include deep breathing exercises, the use of a spirometerAn apparatus for measuring the movement of air into and out of the lungs to encourage deep breathing and expand the lungs, and medicines to help open the airways. In addition, pulmonary rehabilitationBehavior and lifestyle changes to help patients with chronic lung disease decrease breathing problems, return to daily activities, and improve quality of life offers techniques to improve lung function after lung surgery. For example, pursed-lip breathing decreases how often a patient takes breaths and keeps airways open longer. This allows more air to flow in and out of the lungs so that a patient can be more physically active. If respiratory treatments are not prescribed, the patient should ask his or her doctor for a consultation.12,16,17,18
A patient should expect to feel short of breath after lung surgery. The extent of this depends on how much of the lung was removed and how much pain the patient is experiencing. After a portion of a lung is removed, the remaining lung tissue can expand over time and make it easier to breathe. A respiratory therapist can help the patient with breathing treatments after surgery. These treatments may include deep breathing exercises, the use of a spirometerAn apparatus for measuring the movement of air into and out of the lungs to encourage deep breathing and expand the lungs, and medicines to help open the airways. In addition, pulmonary rehabilitationBehavior and lifestyle changes to help patients with chronic lung disease decrease breathing problems, return to daily activities, and improve quality of life offers techniques to improve lung function after lung surgery. For example, pursed-lip breathing decreases how often a patient takes breaths and keeps airways open longer. This allows more air to flow in and out of the lungs so that a patient can be more physically active. If respiratory treatments are not prescribed, the patient should ask his or her doctor for a consultation.12,16,17,18 -
Loss of muscle: Patients benefit from exercise post-surgery. Physical therapy may also be prescribed to help build strength and endurance to overcome post-surgical muscle atrophy.19
What are the risks of lung cancer surgery?
Lung cancer surgery carries risks like any surgery, including:5
- Bleeding
- Infection
- Blood clot
- Allergic reaction to anesthesia medications
- Death
Other risks that specifically may occur after lung surgery include:9
- Failure of the lung to expand
- Injury to the lungs, heart, or blood vessels
- Persistent pain
- Pneumothorax (air or air collection in the space that separates the lung from the chest)
- Pleural effusion (fluid collection in the space around the lung in the chest)
- Pneumonia (bacterial infection in one of the remaining lobes of the lungs)
Updated February 19, 2021
References
- Brunelli A, Postmus PE. Chapter 26: Preoperative Functional Evaluation of the Surgical Candidate. In Pass HI, Ball D, Scagliotti GV, eds. IASLC Thoracic Oncology, Second Edition. Philadelphia, PA: Elsevier, 2018: 265-273. Accessed July 11, 2019.
- Lung Cancer: Early and Locally Advanced—Non-Small Cell Lung Cancer. Version 3.2019, NCCN Guidelines for Patients. https://www.nccn.org/patients/guidelines/lung-early-stage. Posted January 18, 2019. Accessed February 19, 2021.
- Lung Cancer - Small Cell: Types of Treatment. Cancer.Net website. https:k//www.cancer.net/cancer-types/lung-cancer-small-cell/types-treatment. Approved July 2019. Accessed Feberuary 19, 2021.
- Lung Cancer - Non-Small Cell: Treatment Options. Cancer.Net website. http://www.cancer.net/cancer-types/lung-cancer-non-small-cell/types-treatment. Approved May 2020. Accessed February 19, 2021.
- Surgery for Non-Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/non-small-cell-lung-cancer/treating/surgery.html. Revised October 12, 2019. Accessed February 19, 2021.
- Asamura H, Grunenwald D. Chapter 29: Extent of Surgical Resection for Stage 1 and II Lung Cancer. In: Pass HI, Ball D, Scagliotti GV, eds. IASLC Thoracic Oncology, Edition 2. Philadelphia, PA: Elsevier. 2018: 289-294. Accessed July 11, 2019.
- Surgery for Lung Cancer. Memorial Sloan Kettering Cancer Center website. https://www.mskcc.org/cancer-care/types/lung/treatment/surgery. Copyright 2021. Accessed February 19, 2021.
- Thoracotomy. CHEST Foundation website. https://foundation.chestnet.org/patient-education-resources/thoracotomy/. Reviewed May 7, 2020 . Accessed February 19, 2021.
- Lung surgery. Icahn School of Medicine at Mount Sinai website. https://www.mountsinai.org/health-library/surgery/lung-surgery. Copyright 2021. Accessed February 19, 2021.
- Suda, T. Usefulness of robot-assisted surgery for lung cancer demonstrated from the patient's perspective. J Thorac Dis. 2018 Mar. 10(3): 1227-1229. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5906335/. Accessed February 19, 2021.
- Bryant A, Veronesi G, Cerfolio R. Section 28: Robotic Surgery: Techniques and Results for Resection of Lung Cancer. In Pass HI, Ball D, Scagliotti GV, eds. IASLC Thoracic Oncology, Second Edition. Philadelphia, PA: Elsevier. 2018: 283-288. Accessed February 19, 2021.
- Your Lung Operation: Education for a Better Recovery booklet. Surgical Patient Education. American College of Surgeons. https://www.sts.org/sites/default/files/lungbooklet.pdf Accessed February 19, 2021.
- Fatigue. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/fatigue. Approved April 2020. Accessed February 19, 2021.
- Fatigue (PDQ®)—Patient Version. National Cancer Institute website. https:cancer.gov/about-cancer/treatment/side-effects/fatigue/fatigue-pdq. Updated May 15, 2019. Accessed February 19, 2021.
- Chest tube insertion. Medline Plus website. https://medlineplus.gov/ency/article/002947.htm. Reviewed February 8, 2021. Accessed February 19, 2021.
- Shortness of Breath. American Cancer Society website. https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/shortness-of-breath.html. Revised February 1, 2020. Accessed February 19, 2021.
- Deep breathing after surgery. U.S. National Library of Medicine MedlinePlus website. https://medlineplus.gov/ency/patientinstructions/000440.htm. Reviewed September 29, 2019. Accessed February 19, 2021.
- Pulmonary Rehabilitation. National Heart, Lung, and Blood Institute website. https://www.nhlbi.nih.gov/health-topics/pulmonary-rehabilitation. Accessed February 19, 2021.
- Cavalheri V, Burtin C, et al. Exercise training after lung surgery for people with non-small cell lung cancer. Cochrane website. https://www.cochrane.org/CD009955/LUNGCA_exercise-training-after-lung-surgery-people-non-small-cell-lung-cancer#:~:text=Our%20results%20showed%20that…. Published June 17, 2019. Accessed February 19, 2021.
