Discussed in this section is traditional, or standard, chemotherapyTreatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. Chemotherapy is a treatment that uses drugs to stop the growth and division of tumor cells. While each patient responds differently to chemotherapy drugs, chemotherapy treatment can shrink lung cancer tumors, alleviate lung cancer symptoms, and extend life. Chemotherapy can be used at all stagesThe extent of cancer in the body of lung cancer and for both non-small cell lung cancer (NSCLC)A group of lung cancers that are named for the kinds of cells found in the cancer and how the cells look under a microscope and small cell lung cancer (SCLC)An aggressive (fast-growing) cancer that forms in tissues of the lung and can spread to other parts of the body. The cells look small and oval-shaped when looked at under a microscope..
 To help you understand and share this information, you can request our free booklet that summarizes the detailed information in the following sections.
To help you understand and share this information, you can request our free booklet that summarizes the detailed information in the following sections.
Chemotherapy has been used as a cancer treatment for many years and remains important despite the addition in recent years of newer types of drug treatment—targeted therapiesA type of treatment that uses drugs to identify and attack specific types of cancer cells with less harm to normal cells, angiogenesis inhibitorsDrugs given during cancer treatment to prevent the growth of new blood vessels that tumors need to grow, and immunotherapyA type of therapy that uses substances to stimulate or suppress the immune system to help the body fight cancer, infection, and other diseases—that attack cancer in a different way. Chemotherapy may be used as a single drug or in combination with other chemotherapy drugs, in combination with some of the newer treatments, and with surgery and radiation therapyThe use of high-energy radiation from X-rays, gamma rays, neutrons, protons, and other sources to kill cancer cells and shrink tumors to make them more effective.1 Your healthcare team will help to select the best treatment based on your medical history, your overall health and any other medical problems, the stage of your lung cancer, and your preferences.
How does chemotherapy work?
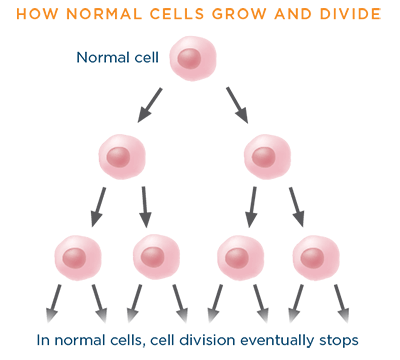
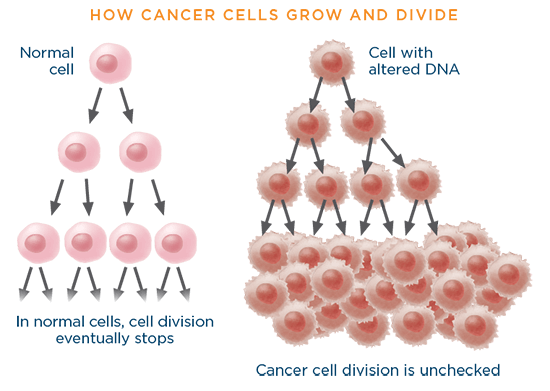
Our bodies are composed of trillions of individual cells, the "building blocks" of life. These cells—of which there are many types serving different functions in the body—have a natural life cycle. Cells that die or are old or damaged are replaced by new cells, through a process by which a living cell duplicates its contents and then divides to form two identical cells. Specifically, within each cell is the nucleusThe central part of most cells that contains genetic material and is enclosed in a membrane, which is comparable to the "brain" of the cell. The nucleus contains chromosomesPart of a cell that contains genetic information (DNA), which are made up of genesCoded instructions within a cell that control how the cell grows in a systematic and precsie way. Genes contain DNA.. Genes, in turn, are made up of DNAThe molecules inside cells that carry genetic information and pass it from one generation to the next. Also called deoxyribonucleic acid., the instructions within a cell that control how the cell grows in a systematic and precise way. Once a cell copies its gene, it divides, forming two new cells, each with its own complete set of genes.2
Healthy, normal cells grow and divide in an orderly manner, per the instructions encoded in the genes, to replace dead, old, or damaged cells.
When a gene has an alteration in its DNA code of instructions, it is said to be "mutated." MutationsAny change in the DNA or gene sequence of a cell. Certain mutations may lead to cancer. occur often, and normally the body can correct them. The correction method is similar to a "spell check" function on a computer or cell phone. However, sometimes the "spell check" function does not work as it should, and the DNA mutation may become part of the cell's blueprint. Over time, an accumulation of mutations can cause cells to lose the capacity to grow and divide in an orderly manner. Out-of-control growth may occur instead, which can lead to the formation of a tumor.3
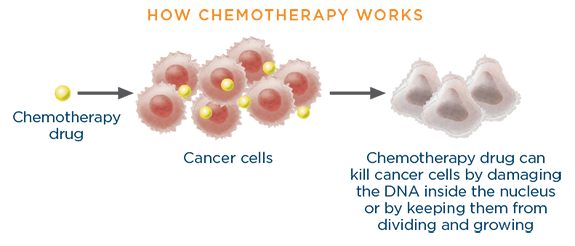
Chemotherapy drugs work by damaging the DNA inside the nucelus of rapidly gowing cells or by keeping the cells from dividing and growing. This may happen either when a cancer cell is making copies of its gene or when the cancer cell is about to divide.2
How chemotherapy drugs differ from targeted therapy and immunotherapy drugs
Chemotherapy drugs are most often used systemically; that is, they travel throughout the whole body (the system) via the bloodsteam to reach and attack cancer cells wherever they may be. However, chemotherapy attacks not just fast-growing cancer cells but also fast-growing healthy cells. Targeted therapy drugs, each of which is intended to treat cancer that has a particular mutation, are aimed at specific signaling pathwaysA group of molecules in a cell that work together to control one or more cell functions that cancer cells use to thrive, blocking them in the same way that blocking a car's fuel line would keep it from running properly. Targeted therapies are more precise than chemotherapy drugs, which may make them more effective. However, not all cancers have a mutation that has a matching targeted therapy.
Immunotherapy drugs do not attack cancer cells directly; they work by strengthening the body's own immune system's ability to recognize cancer cells and selectively target and kill them.4,5
How is chemotherapy administered?
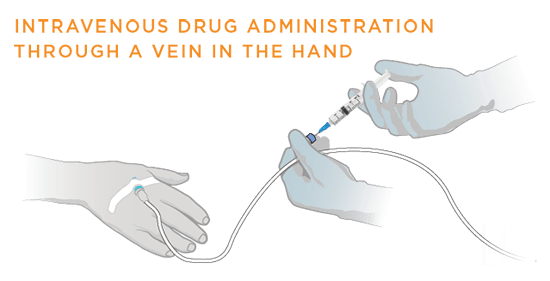
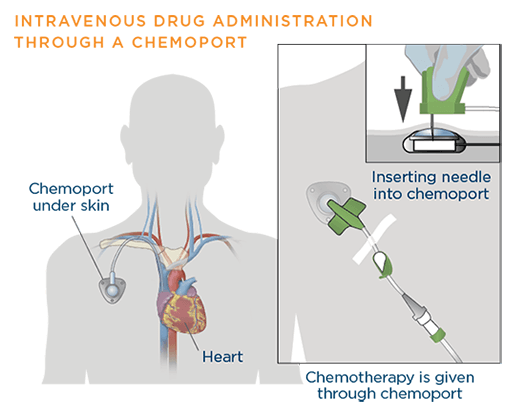
Chemotherapy can be administered systemically in many ways, including orally, intravenouslyThrough a needle or tube inserted into a vein, subcutaneouslyBeneath the skin, and intramuscularlyWithin a muscle. To treat lung cancer, chemotherapy drugs are usually given intravenously—through a needle or tube inserted into a vein.6

Sometimes a chemoportA device used to deliver the chemotherapy drug. It is placed under the skin, usually in the chest, and attached to a catheter that is guided into a large vein, the superior vena cava, above the right side of the heart. may be placed under the skin. The chemoport may stay for a few weeks to months and helps in the administration of the chemotherapy drug while avoiding multiple needle pricks.7
The way the chemotherapy is given depends on the type and stage of the cancer being treated. Most often, chemotherapy is given systemically; this process is described here.
Chemotherapy may be given one drug at a time or as a combination of different drugs at the same time. Usually chemotherapy is given in cycles. A typical cycle consists of a period of treatment of 1 to 3 days, followed by a break before the next treatment is given so that a patient can rest and allow the body time to recover. A chemotherapy cycle generally lasts 3 to 4 weeks and continues over a period of months. Sometimes chemotherapies are planned for a specific number of cycles, typically 4-6 cycles. In other situations, chemotherapy is planned to be continual—on an ongoing basis as long as it is tolerated and controlling the cancer.8,9
The number of treatments within a cycle, the length of a cycle, and the number of cycles to be given may vary based on the type and stage of lung cancer and the drug(s) being given. It is always a good idea for you to check with your healthcare team to understand your treatment plans, including:
- What drugs are being used
- The drug schedule
- The length of a cycle
- How many cycles are planned
- What to expect between cycles
Preparing for chemotherapy treatment
There are a number of things you can do to help prepare for chemotherapy treatment. Your healthcare team will advise you on these. They may include:10,11,12
- Having a surgcal procedure to insert a device, such as a chemoport, into a vein if your chemotherapy will be administered intravenously. The advantage of this is that a vein will not need to be found at each chemotherapy session
- Going to your dentist to make certain that there is no existing infection that could complicate your treatment and having any necessary dental work done prior to starting treatment
- Planning ahead for possible side effects. Side effects and how to alleviate them will be discussed further along in this section
- Arranging for transportation and help around the house. You may or may not need the help, but it is not possible to predict before your treatment begins
- Getting a checklist from your healthcare team about what to expect before, during, and after chemotherapy
Goals of lung cancer chemotherapy
The goals of lung cancer chemotherapy depend on the type of lung cancer being treated, the stage of the lung cancer, and whether other types of treatment will be given. Some possible goals of chemotherapy are:
- To eliminate all of the cancer cells and to prevent recurrence after surgery or some other type of treatment
- To decrease the size of tumors for easier and safer removal by surgery
- To control the lung cancer by stopping it from growing and spreading
- To help make other cancer-killing treatments, such as radiation therapy, more effective
- To relieve symptoms caused by the cancer and to slow its growth when the lung cancer is at an advanced stage. This type of treatment is called palliative careCare given to improve the quality of life of patients who have a serious or life-threatening disease1,13
Commonly used chemotherapy drugs
Commonly used chemotherapy drugs to treat NSCLC include:14,15,16
| Generic (chemical) name | Brand Name (sold as) |
| Carboplatin | Paraplatin® |
| Cisplatin | Platinol-AQ® |
| Docetaxel | Taxotere® |
| Etoposide | Etopophos® |
| Gemcitabine | Gemzar® |
| Paclitaxel | Taxol®, Onxol® |
| Paclitaxel (albumin-bound) | Abraxane® |
| Pemetrexed | Alimta® |
| Vinorelbine | Navelbine® |
When combination chemotherapy is used (because the drugs work in different ways and may be more effective together), usually it is the drugs made with platinum—carboplatin (Paraplatin®) and cisplatin (Platinol-AQ®)—that are used with another drug.14
Commonly used chemotherapy drugs to treat SCLC include:17
| Generic (chemical) name | Brand Name (sold as) |
| Carboplatin | Paraplatin® |
| Cisplatin | Platinol-AQ® |
| Etoposide | Etopophos® |
| Ironotecan | Camptosar® |
| Lurbinectedin | ZepzelcaTM |
| Topotecan | Hycamtin® |
Combination chemotherapy is usually the main treatment for patients with SCLC as the first round of chemotherapy. As with NSCLC, the combinations are most often a platinum-based drug (carboplatin [Paraplatin®] or cisplatin [Platinol-AQ®]) that is combined with another drug; cisplatin (Platinol-AQ®) and etoposide (Etopophos®) is most often the first combination chemotherapy used.17 There is another chemotherapy drug used specifically for adult patients with extensive-stage SCLC whose cancer has progressed on or after platinum-based chemotherapy. This is lurbinectedin (ZepzelcaTM).20
When is chemotherapy given for lung cancer?
Chemotherapy is among the treatment options, but never the only option, at all stages of both NSCLC and SCLC. Note that treatment options develop over time; your healthcare team may suggest other options that are not outlined below.
When given along with other treatments, the chemotherapy is referred to as advjuvant, neoadjuvant, or concurrent.
- Adjuvant chemotherapy: After surgery or radiation therapy, there may still be some microscopic cancer cells left behind that cannot be seen on regular computed tomography (CT) scansProcedure that uses a computer linked to an X-ray machine to make a series of detailed pictures of areas inside the body. When chemotherapy is given to kill those microscopic cancer cells, it is called adjuvant chemotherapy.
- Neoadjuvant chemotherapy: Chemotherapy may be given before surgery to shrink the cancer and make it easier to remove with surgery, in addition to killing cancer cells that cannot be seen on regular CT scans. This is called neoadjuvant chemotherapy. Sometimes neoadjuvant chemotherapy is given along with radiation therapy.
- Concurrent chemotherapy: When chemotherapy is given at the same time as radiation therapy, it is called concurrent chemotherapy, or sometimes concurrent chemoradiotherapy. Concurrent treatment may be given as the only planned therapy or it may be given in the neoadjuvant setting before a planned surgery.14,17
Chemotherapy treatment options for non-small cell lung cancer (NSCLC), by stage
In NSCLC, chemotherapy may be used as the main treatment, but it is also frequently given along with other treatments.
Stage 1 and stage II NSCLC: Your healthcare team may recommend adding chemotherapy to your surgical treatment plan. Chemotherapy may be given as neoadjuvant chemotherapy to reduce the size of the tumor or as adjuvant chemotherapy to reduce the risk of the cancer coming back.18,23
Stage III NSCLC: Chemotherapy is frequently used in stage III treatment, either alone or in combination with external beam radiation therapy (EBRT), a type of radiation therapy. In those cases where surgery is performed, chemotherapy may precede or follow it, either with or without radiation.19,23
Stage IV NSCLC: Treatment of stage IV NSCLC patients with chemotherapy depends on the performance status of a patient and whether their cancer has a driver mutationA change in the DNA of a gene that leads to the development or progression of a tumor (as determined by biomarker testingAnalyzing DNA to look for a gene mutation that may indicate an increased risk for developing a specific disease or disorder). Your healthcare team will use one of several scales, such as the Eastern Cooperative Oncology Group (ECOG) Performance Scale, to measure your general health to help determine which treatments, including chemotherapy, that may be the best for you.21,22
| ECOG Performance Score | Definition |
| 0 | Patient is fully active and able to carry on all pre-disease performance without restriction |
| 1 | Patient is restricted in physically strenuous activity but ambulatory (able to walk and not confined to bed) and able to carry out work of a light or sedentary nature, e.g., light housework or office work |
| 2 | Patient is ambulatory and capable of all self-care but unable to carry out any work activities: the patient is up and about more than 50% of waking hours |
| 3 | Patient is capable of only limited self-care. The patient is confined to bed or chair more than 50% of waking hours |
| 4 | Patient is completely disabled, cannot carry on any self-care, and is totally confined to bed or chair |
Some patients' performance scores improve after initial treatment, making them eligible for additional treatments.
Chemotherapy treatment options for patients with stage IV NSCLC may include:23
- combination chemotherapy
- combination chemotherapy and targeted therapy with a monoclonal antibodyA type of protein made in the laboratory that can bind to substances in the body, including cancer cells.. It can be used alone or to carry drugs, toxins, or radioactive substances directly to cancer cells, e.g., necitumumab
- chemotherapy with immunotherapy
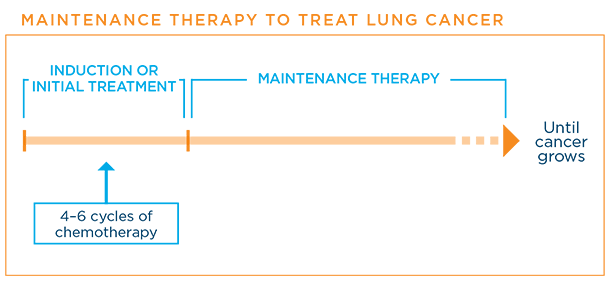
Depending on your health and response, your healthcare team will make recommendations for maintenanceTreatment that is given to help keep cancer from coming back after it has disappeared following the initial therapy or second-lineTreatment that is given when initial treatment (first-line therapy) doesn't work or stops working or further therapy.
Maintenance treatments may include the same or other chemotherapies or simply a "watch and wait" approach. The goal of maintenance therapy is to help keep the cancer from growing again. Generally, a patient is kept on maintenance therapy as long as the cancer stays controlled.24
Chemotherapy treatment options for SCLC, by stage
In small cell lung cancer (SCLC), for which there are fewer treatment options than in NSCLC, chemotherapy is usally the main treatment for two reasons:
- SCLC responds initially very well to chemotherapy
- SCLC may spread quickly beyond the lungs. Chemotherapy is the best option to initially treat cancer that has spread, so it is given in almost all SCLC cases, even if there is no sign of spread on CT scans.16
For limited-stage SCLCSCLC found in one lung, the tissues between the lungs, and nearby lymph nodes only, your healthcare team may recommend these chemotherapy options:37
- chemotherapy following surgery
- chemotherapy and radiation therapy following surgery
For extensive-stage SCLCSCLC therapy to the head to reduce the risk that cancer will spread to the brain, your healthcare team may recommend these chemotherapy options:37
- combination chemotherapy
- combination chemotherapy and immunotherapy
- chemotherapy followed by radiation therapy
Why there are side effects from chemotherapy drugs
Chemotherapy drugs kill rapidly dividing cells and cannot tell the difference between rapidly growing cancer cells and healthy, normal cells that also divide rapidly. Most healthy, normal cells do not divide rapidly. Those that do include hair cells, blood cells (red blood cellsA type of blood cell that carries oxygen from the lungs to all parts of the body, plateletsA type of blood cell responsible for blood clotting, and white blood cellsA type of blood cell that helps the body fight infection and other diseases), and the cells lining the mouth and intestines. When chemotherapy attacks these healthy, normal cells, it can cause side effects. However, normal cells can repair the damage or be replaced by other healthy cells, which is why side effects are usually temporary.38
Common side effects of lung cancer chemotherapy
The most common side effects of chemotherapy in both NSCLC and SCLC are:25,38
Note: Each chemotherapy drug has a different set of most common side effects. Likewise, each person differs in their response to chemotherapy. Just because a side effect is possible doesn’t mean that you will experience it.
- Constipation
- Diarrhea
- Easy bruising or bleeding: Due to a low number of blood platelets (thrombocytopenia)
- Fatigue
- Hair loss
- Increased risk of infection: Due to a low number of white blood cells (neutropenia)
- Loss of appetite
- Change in taste
- Mouth and throat sores
- Nausea, vomiting
- Peripheral neuropathy: A nerve problem that causes pain, burning or tingling sensations, sensitivity to cold or heat, or weakness, mainly in the hands and feet
While most of the side effects of chemotherapy stop after treatment, some side effects may continue, recur, or develop later. Among the serious long-term effects may be heart disease, another type of cancer, low levels of thyroid hormones, fertility issues, and cognitiveRelating to conscious intellectual activity, such as thinking, reasoning, or remembering problems. These can occur even years after treatment is completed. For that reason, it is essential if you receive chemotherapy that you are followed up throughout your life by a healthcare team that is aware of the potential side effects of treatment.25,38
Managing the side effects of lung cancer chemotherapy
When I was told I had cancer, one of the first images that popped into my head was of me being bald and frail from chemo. So one of the biggest lessons for me has been that the chemo with which I was treated doesn't cause the side effects I had come to associate with cancer treatment.
—C.K., survivor with NSCLC
It is important to discuss each chemotherapy drug with your healthcare team to be prepared for potential side effects and to understand what can be done to treat them. The healthcare team can often prescribe drugs or make recommendations about other ways to help relieve and/or prevent many of these side effects. Be sure to communicate with the healthcare team if and when new side effects begin, as treating them early on is often more effective than trying to treat them once they have already become severe. Sometimes the doses of the chemotherapy drugs may need to be lowered or treatment may need to be delayed to prevent the side effects from being worse.
Some specific ways in which the common side effects of chemotherapy drugs are sometimes managed are listed below; this list is by no means comprehensive. Again, discuss side effects with your healthcare team to determine the best approaches to managing them given your particular situation.
- Constipation: Stool softeners, laxatives26
- Diarrhea: Ani-diarrheal medications27
- Easy bruising or bleeding: Lower chemotherapy dose; longer time between chemotherapy cycle; platelet transfusion28
- Fatigue: Treat underlying condition that contributes to the fatigue. For example, if fatigue is related to depression, antidepressant medications29
- Hair loss: Cold cap therapyWearing a cap or head covering with cold packs before, during, or after chemotherapy to help prevent hair loss. The cold narrows the blood vessels in the skin on the head, which means that less of the drug reaches the hair follicles, the small openings on the scalp through which hair grows; medications; emotional support; cranial prosthesisA wig custom-made after hair loss from a condition or a treatment, such as chemotherapy30
- Increased rate of infection: Preventive antibiotics; washing hands well; using lotion to keep skin from cracking; avoiding people with contagious illness; take filgrastim (Neupogen®), a medication that increases the number of infection-fighting cells in the body31
- Loss of appetite: Eating five or six small meals a day; eating as much as want; increase calories to food (e.g., add butter); taking appetite stimulants or nutritional supplements n to improve appetite and reduce weight loss.32
- Taste changes: Choosing foods that appeal, even if new; using plastic untensils; using glass cookware33
- Mouth and throat sores: Rinsing/gargling with a solution of salt water and baking soda; avoidance of foods that are spicy, salty, or acidic34
- Nausea, vomtiing: Medications, including both preventive and therapeutic: IV fluids, behavioral therapy35
- Peripheral neuropathy: Physical therapy or complementary therapies (such as massage and acupuncture); medications (for neuropathic pain), including anticonvulsants and antidepressants; over-the-counter pain medications for mild pain; prescription non-steroidal anti-inflammatory drugsA class of drugs that reduce pain, fever, and inflammation for severe pain; diet rich in B1 and B12, folic acid, and antioxidantsA substance that protects cells from the damage caused by free radicals, unstable molecules made by the process of oxidation during normal metabolism36
What clinical trial options are available?
If you are considering participating in a clinical trial, start by asking your healthcare team whether there is one that might be a good match for you in your geographic area. In addition, here are several resources to help you find one that may be a good match:
- EmergingMed: 877-769-4834, https://app.emergingmed.com/lcctal/home
- National Cancer Institute website: www.cancer.gov/clinicaltrials/search
- My Cancer Genome: www.mycancergenome.org/
- Lung Cancer Master Protocol (Lung-MAP): www.lung-map.org
Learn more about clinical trials here.
Updated March 5, 2021
References
- Hellman MD, et al. Chemotherapy remains an essential element of personalized care for persons with lung cancer. Ann Onc 2016 Oct 27(10):1829-1835. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5035786/. Published July 25, 2016. Accessed February 23, 2021.
- Chemotherapy works. Cancer Research UK website. https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/chemotherapy/how-chemotherapy-works. Reviewed June 10, 2020. Accessed February 23, 2021.
- The Genetics of Cancer. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/cancer-basics/genetics/genetics-cancer. Approved March 2018. Accessed February 23, 2021.
- The Differences between Chemotherapy and Targeted Therapy. Sino Biological website. https://www.sinobiological.com/the-differences-between-chemotherapy-and-targeted-therapy.html. Copyright 2021. Accessed February 23, 2021.
- Targeted Cancer Therapies. National Cancer Institute website. https://www.cancer.gov/about-cancer/treatment/types/targeted-therapies/targeted-therapies-fact-sheet#:~:text=Targeted%20therapies%20differ%20from%20s…. Updated January 25, 2021. Accessed February 23, 2021.
- How is Chemotherapy Given? Chemocare.com website. https://chemocare.com/chemotherapy/what-is-chemotherapy/how-chemotherapy-is-given.aspx. Copyright 2021. Accessed February 23, 2021.
- Catheters and Ports in Cancer Treatment. Cancer.Net website. https:///www.cancer.net/navigating-cancer-care/how-cancer-treated/chemotherapy/catheters-and-ports-cancer-treatment. Approved December 2020. Accessed February 23, 2021.
- Chemotherapy for Non-Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/non-small-cell-lung-cancer/treating/chemotherapy.html. Revised May 27, 2020. Accessed February 23, 2021.
- Chemotherapy for Small Cell Lung Cancer. American Cancer Society website. https://www.cancer.org/cancer/small-cell-lung-cancer/treating/chemotherapy.html. Revised February 17, 2021. Accessed February 23, 2021.
- Chemotherapy. Mayo Clinic website. https://www.mayoclinic.org/tests-procedures/chemotherapy/about/pac-20385033. Copyright 2021. Accessed February 23, 2021.
- What to Expect When Having Chemotherapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/chemotherapy/what-expect-when-having-chemotherapy. Approved June 2019. Accessed February 23, 2021.
- Chemotherapy Before, During, and After. American Lung Association website. https://www.lung.org/getmedia/b2ddb6a5-7ff0-465a-b7ac-546055fdec16/chemotherapy-worksheet-1.pdf.pdf. Accessed February 23, 2021.
- Understanding Chemotherapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/chemotherapy/understanding-chemotherapy. Approved May 2019. Accessed February 23, 2021.
- Drugs Approved for Lung Cancer. National Cancer Institute website. https://www.cancer.gov/about-cancer/treatment/drugs/lung. Updated January 19, 2021. Accessed February 23, 2021.
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Non-Small Cell Lung Cancer. Version 4.2021. National Comprehensive Cancer Network, Inc. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Posted February March 3, 2021. Accessed March 4, 2021.
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Small Cell Lung Cancer. Version 2.2021. National Comprehensive Cancer Network, Inc. https://www.nccn.org/professionals/physician_gls/pdf/sclc.pdf. Posted January 11, 2021. Accessed February 23, 2021.
- Lung Cancer — Small Cell: Types of Treatment. Cancer.Net website. https:/k/www.cancer.net/cancer-types/lung-cancer-small-cell/types-treatment. Approved July 2019. Accessed February 23, 2021.
- How is Chemotherapy Used to Treat Cancer? American Cancer Society website. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/how-is-chemotherapy-used-to-treat-cancer.html. Revised November 22, 2019. Accessed February 23, 2021.
- Radiation Therapy for Non-Small Cell Lung Cancer. American Cancer Society website https://www.cancer.org/cancer/non-small-cell-lung-cancer/treating/radiation-therapy.html. Revised October 1, 2019. Accessed February 23, 2021.
- ZepzelcaTM (lurbinectedin) [package insert] Jazz Pharmaceuticals, Inc. Palo Alto, CA. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213702s000lbl.pdf Revised June 2020. Accessed March 5, 2021.
- ECOG Performance Status. ECOG-ACRIN Cancer Research Group website. https://ecog-acrin.org/resources/ecog-performance-status. Copyright 2020. Accessed March 5, 2021.
- Lung Cancer: Metastatic—Non-Small Cell Lung Cancer. Version 3.2019. NCCN Guidelines for Patients®. https://www.nccn.org/patients/guidelines/content/PDF/lung-metastatic-patient.pdf. Posted January 18, 2019. Accessed March 5, 2021.
- Non-Small Cell Lung Cancer Treatment (PDQ®)—Patient Version. National Cancer Institute website. https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment.pdq. Updated December 3, 2020. Accesssed March 1, 2021.
- Understanding Maintenance Therapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/understanding-maintenance-therapy#:~:text=Maintenance%20therapy%20is%20used%20for,ca…. Approved May 2019. Accessed March 5, 2021.
- Side Effects of Chemotherapy. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/chemotherapy/side-effects-chemotherapy. Approved August 2019. Accessed March 5, 2021.
- Constipation. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/side-effects/constipation. Approved December 2019. Accessed March 5, 2021.
- Diarrhea. Cancer.Net website. https://www.cancer.net/navigating-cancer-care/side-effects/diarrhea. Approved December 2020. Accessed March 5, 2021.
- Low Platelet Count or Thrombocytopenia. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/low-platelet-count-or-thrombocy…. Approved August 2020. Accessed March 5, 2021.
- Fatigue. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/fatigue. Approved April 2020. Accessed March 5, 2021.
- Hair Loss or Alopecia. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/hair-loss-or-alopecia. Approved January 2020. Accessed March 5, 2021.
- Infection. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/infection. Approved February 2020. Accessed March 5, 2021.
- Appetite Loss. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/appetite-loss. Approved April 2020. Accessed March 5, 2021.
- Taste Changes. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/taste-changes. Approved January 2020. Accessed March 5, 2021.
- Mouth Sores or Mucositis. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/mouth-sores-or-mucositis. Approved January 2020. Accessed March 5, 2021.
- Nausea and Vomiting. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/nausea-and-vomiting. Approved July 2020. Accessed March 5, 2021.
- Nerve Problems or Neuropathy. Cancer.Net website. https://www.cancer.net/coping-with-cancer/physical-emotional-and-social-effects-cancer/managing-physical-side-effects/nerve-problems-or-neuropathy. Approved October 2018. Accessed March 5, 2021.
- Small Cell Lung Treatment (PDQ®)—Patient Version. Natioinal Cancer Institute website. https://www.cancer.gov/types/lung/hp/small-cell-lung-treatment-pdq. Updated May 21, 2020. Accessed March 5, 2021.
- Chemotherapy Side Effects. American Cancer Society website. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/chemotherapy-side-effects. Reviewed May 1, 2020. Accessed March 5, 2021.
